
Radiotherapy
Radiotherapy uses radiation beams to treat and destroy cancer cells. Both external and internal radiotherapy can be used to treat prostate cancer.

Radiotherapy uses radiation beams to treat and destroy cancer cells. Both external and internal radiotherapy can be used to treat prostate cancer.
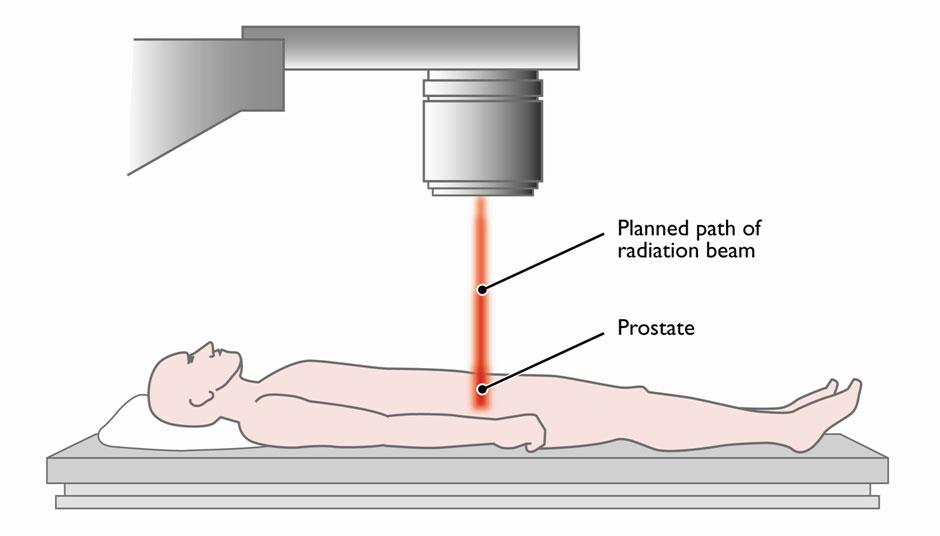
External beam radiotherapy can be used to treat T1, T2 and T3 prostate cancer.For cancer that is localised to the prostate it is usual for a type of treatment called hormone therapy to be give a few months before radiotherapy starts. This reduces the size of the prostate and makes it more easier to treat. The treatment will stop after radiotherapy has been completed. More information on hormone therapy can be found here
If T3 (locally advanced) disease is present, hormonal therapy may be continued for two to three years afterwards. External beam radiotherapy usually takes two to six weeks of treatment, every day, five days a week, for around 10 minutes a day.
Before starting external beam radiotherapy, a CT scan will be performed to help visualise the area to be treated. This area may be marked with a small medical tattoo.
Sometimes breathing can cause the prostate gland to move slightly which may make it difficult to focus the radiotherapy. If the prostate moves 6mm out of position, radiotherapy may miss the prostate and affect tissue around it.
The medical team may therefore recommend that three small gold markers (about 2mm in size) called fiducial markers are inserted into the prostate before radiotherapy. This allows more accurate targeting of the prostate even if it moves slightly. These markers will remain in the prostate permanently but should not cause any medical problems.
There are two types of external radiotherapy:
This focuses radiation using 3D computerised imaging to target cancer, reducing the risk of damage to healthy surrounding tissue.
This assesses the shape of the cancer. It increases the dose given to the central part of the tumour and treats the surrounding area with a lower dose.
IMRT is also able to ‘bend’ the radiotherapy beam to avoid damaging structures that should not receive treatment.
It is especially useful for men who have a larger volume of prostate cancer which has spread to the surface of the prostate or seminal vesicles.
A newer type of IMRT can now be delivered using a machine called a rapidarc which rotates around the body. This reduces treatment time and uses a lower overall dose of radiotherapy.
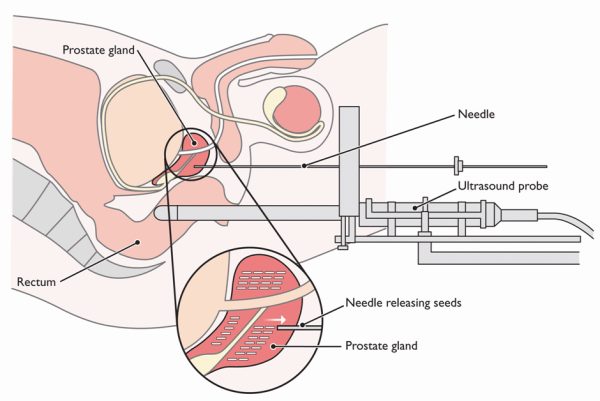
This radiotherapy treatment uses tiny radioactive seeds that can be implanted in the prostate during a minor operation. This is called permanent brachytherapy. These seeds decay and give off radiation which can kill cancer cells. This type of treatment will usually only involve one or two hospital visits and does not usually require the use of hormonal therapy beforehand.
Brachytherapy is usually used to treat T1 and T2 prostate cancer.
For more information on brachytherapy from the British Association of Urology Surgeons (BAUS) please click here.
This type of radiotherapy involves the insertion of radioactive rods into the prostate which are not permanent.
This is where non-permanent brachytherapy is combined with external beam radiotherapy.
There are other radiotherapy techniques which are less common. These are not widely available everywhere in the UK but may be available within the private sector or, in certain circumstances, within the NHS.
This type of radiotherapy uses sophisticated computer imaging techniques to enable a higher dose of radiotherapy to be given reducing the length of treatment needed.
External beam radiation releases its strongest dose of radiation soon after penetrating the skin on its way to the tumour – and again as it passes through and beyond the tumour.
Proton Beam Therapy uses a different type of radiation which can be targeted directly at the tumour site and then stop releasing energy that could go beyond the prostate. It can also release most of its energy at precise depths.
Specialists who support Proton Beam Therapy say it may cause less damage to surrounding healthy tissue.
Proton Beam Therapy has been used for some time for particularly challenging cancers. However, it is not standard practice in the UK for prostate cancer.
Pencil Beam Radiotherapy is a more precise type of proton beam therapy using a very thin beam of radiation to treat prostate cancer.
For general information on radiotherapy from NHS Choices please click here.
Radiotherapy can affect the nerves surrounding the prostate that control erections. There are several treatments for erectile dysfunctionand further information can be found here.
Radiotherapy does not usually cause urinary incontinence. However, sometimes it causes a narrowing of the urethra (the passage that transports urine inside the penis). This may lead to difficulties passing urine. This tends to occur some years after treatment.
In a small number of men, radiotherapy can inflame the lining of the rectum (back passage). This may be temporary but can sometimes be permanent. It can cause bleeding from the back passage or mean men may need to pass stool (poo) more often.
After radiotherapy, men will have regular blood tests to check their PSA level.
If cancer returns following radiotherapy, prostatectomy (removal of the prostate gland) is not recommended. In this situation, newer treatments such as HIFU or Cryosurgery may be offered to control the disease.