
Surgery (Radical Prostatectomy)
Surgery, known as radical prostatectomy, is a common way to treat localised prostate cancer. Occasionally it may be reccomended for more advanced cancer.

Surgery, known as radical prostatectomy, is a common way to treat localised prostate cancer. Occasionally it may be reccomended for more advanced cancer.
During surgery, the whole of the prostate gland and the surrounding seminal vesicles is removed. Prostatectomy is considered a major operation, although men will only be in hospital for a few days.
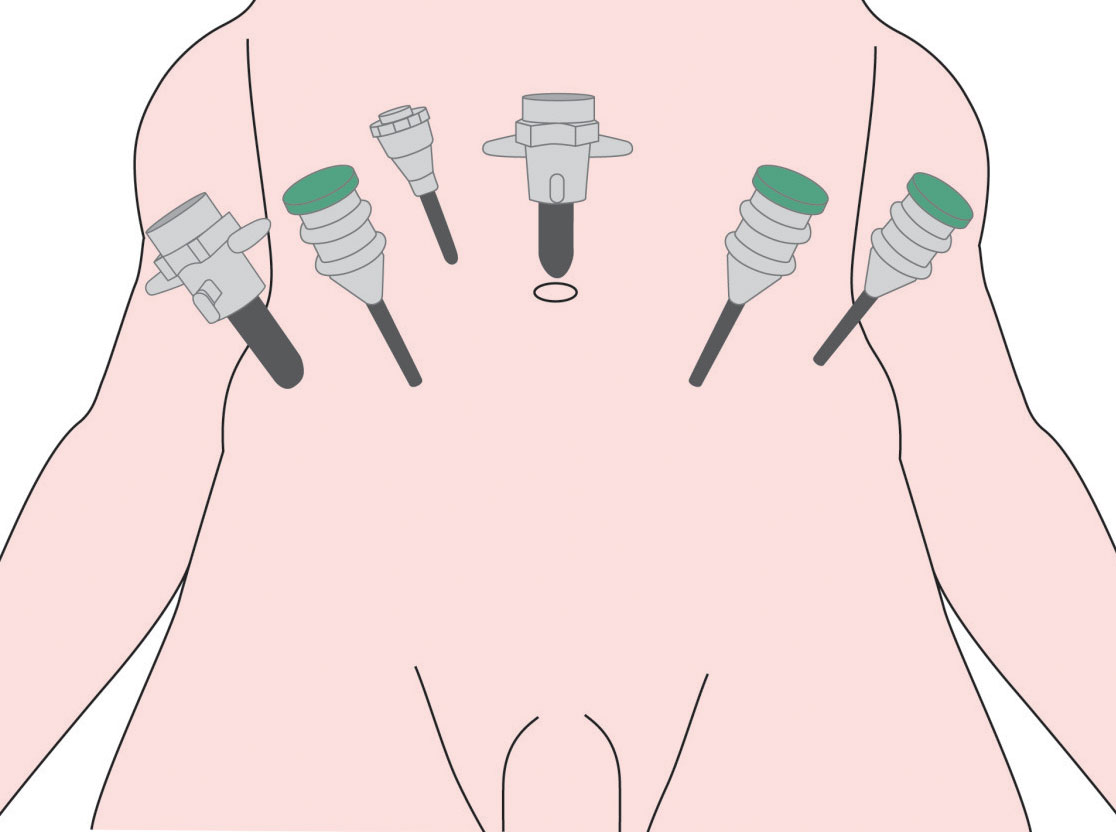
There are several different ways that the procedure can be performed:
If a PSA level is above 10, surgeons may remove nearby lymph nodes to check for any spread of cancer outside the prostate. More information about the lymphatic system and lymph nodes can be found here.
Men should be able to eat and drink straight away and painkillers will be given on a regular basis.
A small plastic tube called a ‘drain’ may be left in the abdomen for a short time after the operation. This is to collect any excess blood draining from the operation site which could accumulate and delay the healing process.
To allow time for the operation site to heal, men will have a urinary drainage tube called a catheter fitted and this will be left in place for up to 10 days.
More information about urinary catheters, how they work and how they should be managed can be found here.
The nerves that control erections are situated very close to the prostate gland. During surgery, these nerves may be affected.
If only a small amount of prostate cancer is present, the surgeon may be able to avoid removing these nerves, a technique called nerve sparing surgery. This means that there is a greater chance that men will regain erections fully, although it may take a year or more to fully improve.
If there is more disease, it is less likely that the surgeon will be able to save these nerves, as the priority will be to ensure that no cancer is left behind.
There are a number of different treatments which can be used following prostatectomy and other treatments which can improve erections. For more information on treatment for Erectile Dysfunction, please see here.
During prostate cancer surgery, the structures which help control urinary continence will be removed. This means that men who have this surgery may suffer from a type of urinary incontinence called stress incontinence. This is where it is hard to control urination and men may find that they leak some urine and need to wear protective pads for a short time after surgery.
Stress incontinence after surgery can be improved by performing pelvic floor exercises. These are explained below.
Urinary symptoms should improve quickly after surgery and return to normal within two to three months. However, a small number of men may find that after a year they still suffer some minor stress incontinence. This will typically happen when they laugh, cough, sneeze or perform sudden movements. Wearing a small pad can catch small accidents and avoid embarrassment.
The ‘pelvic floor’ is a way of describing the layers of muscle that support the bladder and the bowel, stretching from the tailbone at the back to the pubic bone at the front. Doing pelvic floor exercises can help with erections as well as urinary continence after surgery.
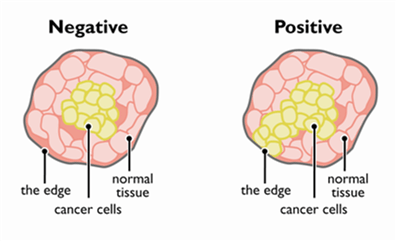
Once the prostate gland has been removed, it is carefully examined under a microscope by scientists called histo-pathologists. They will be able to tell if the cancer was only within the prostate itself and if the surgeon was able to remove it all.
The edges of tissue removed during cancer surgery are called ‘margins’ and ideally, the margins should be free from cancer cells. If there is evidence that there are some cancer cells at the margins but possibly were not spreading beyond it then the medical team will call this a positive margin.
If all the cancer has been removed with the prostate, the PSA level should stay low (at less than 0.1). If it is higher than this, you may need further treatment, usually radiotherapy.
Removing the prostate gland naturally creates a gap between the urethra and the bladder. This is surgically repaired by re-joining the urethra to the bladder with stitches.
Sometimes surgery can cause scar tissue to form at the operation site and narrow the urethra. This can make it difficult to pass urine. This is called a urethral stricture. In this case, minor surgery can be performed to widen the urethra.
After surgery, your Multi Disciplinary Team (MDT) will discuss the results from the operation. As mentioned earlier, if there is a concern that cancer may still be present, a further treatment such as radiotherapy may be suggested.
Men will have outpatient appointments, usually every three months, where PSA levels will be checked. This will gradually increase to six monthly and then yearly.
Click here for more information on prostatectomy from the British Association of Urology Surgeons.