Diagnosis and Orchidectomy
An ultrasound scan is used to identify a testicular lump. If it shows that cancer might be present the testicle will need to be removed by surgery. This operation is called an orchidectomy.
In addition to orchidectomy other tests are performed to determine if the cancer has spread and to help guide treatment decisions. These are usually repeated at regular intervals after surgery and other treatments to monitor response.
| Blood tests | Some testicular cancers release chemical substances into the bloodstream. These are called tumour markers. Alpha-fetoprotein (AFP), human chorionic gonadotrophin (HCG) and lactate dehydrogenase (LDH). They can be abnormal in the presence of certain types of testicular cancer. They can also be used to measure the effect of surgery on reducing cancer activity after orchidectomy. Some men may have a low testosterone level before surgery and treatment may reduce it further. A blood test to check your testosterone level may be performed. |
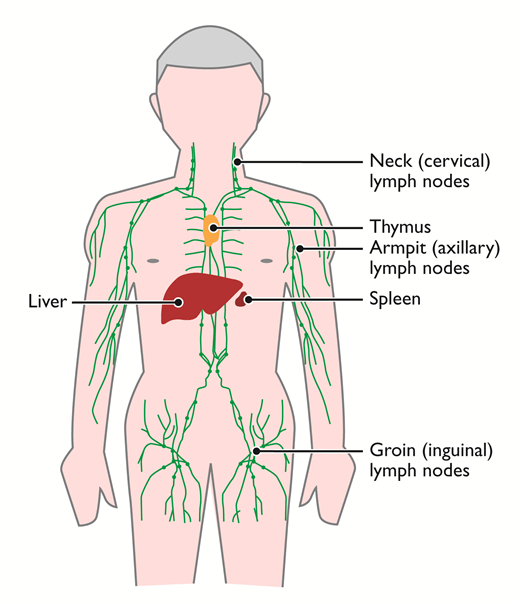
| Computerised Tomography Scan (CT scan) | A CT scan of the chest, abdomen and pelvis is performed to see if cancer has spread to other areas of the body such as the lungs or lymph glands in the abdomen (see below). |
| Sperm Storage | Treatment for testicular cancer may reduce fertility (ability to father a child), and sometimes men will be advised to store sperm before treatment. |
The Lymphatic System and Lymph Nodes
The lymphatic system transports a fluid called lymph. Lymph will contain various cells and substances that the body no longer needs and passes through small oval structures called lymph nodes. These filter out unwanted substances. Cancer can travel in lymph and can spread to other areas of the body.
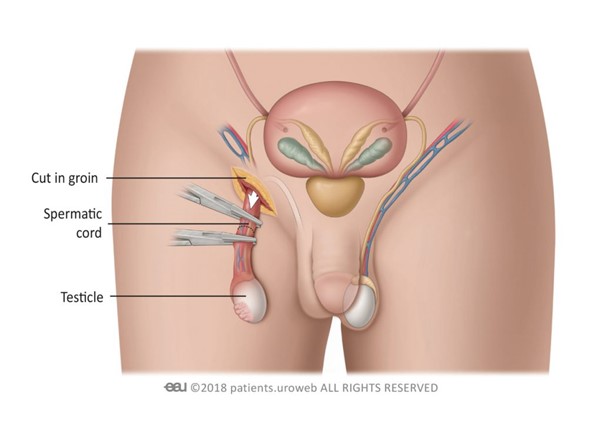
Orchidectomy
An orchidectomy (unilateral), is an operation to remove one testicle. It is carried out under a general anaesthetic, which means you are put to sleep for surgery. During surgery, a small incision is made into the groin region on the affected side and the testicle is removed. The scrotum is not cut. The cancerous testicle will then be sent to a laboratory to be analysed.
After Surgery
- A dressing will cover the incision site on the groin which can be removed after 24 hours. Stitches (sutures) will dissolve but may take a few weeks to disappear.
- You can have a bath or shower after 24 hours, but do not rub soap on the wound area. The area should be dried by gently patting it with a clean towel.
- The groin and scrotal area will feel bruised and swollen after the operation. It is better to wear close fitting underwear, such as briefs or ‘Y’ fronts or a scrotal support rather than boxer shorts. This will help the bruising settle.
- Painkillers should be taken as prescribed on a regular basis.
- Although this is a minor operation, you should reduce strenuous activity for the first week but should be able to return to work within a few weeks.
- Occasionally a collection of blood may form around the wound (haematoma) or it may become infected. You should seek medical advice if the operation site becomes very red or sore which could be signs of infection.
- You should only start driving when you are able to perform an emergency stop without hesitation.
- Sexual activity can begin after two weeks if it feels comfortable to do so.
Having an orchidectomy should not affect your ability to have an erection, but the stress associated with a potential diagnosis of cancer may affect sexual performance.
Prosthetic (artificial) testicle
A prosthetic or artificial testicle is a silicone implant which will resemble a normal testicle. It can be inserted at the time of orchidectomy or if you are unsure that you want one, after your treatment has finished. Once inserted, the neck of the scrotum is sealed with stitches to prevent it from moving up into the groin.
- The cosmetic result may vary. For example, the artificial testicle may not exactly match the size of the normal testicle that remains on the other side.
- Scar tissue can form around the implant inside the scrotum. This can sometimes cause a thickening of tissue which may in turn cause discomfort.
- Although exceptionally rare, rupture of the implant can occur due to vigorous activities such as contact sport, cycling or physical contact including sexual intercourse.
- Sometimes the implant may move out of its original position.
- A prosthetic testicle will not react to temperature like a normal one and will stay the same size.
- If you need chemotherapy treatment after orchidectomy an artificial implant may increase the risk of infection due to a lowered immune system.
What Happens Next?
The MDT (Multi-Disciplinary-Team)
An MDT is a group of medical experts who are managing your care. When the results of surgery, blood tests and scans are available, they will make a recommendation about any further treatment that you may need. Several options may be recommended for further treatment, and these will be discussed with you. For men who have Stage 1 testicular cancer there may be several options such as those below.
| Surgery | Chemotherapy | Radiotherapy |
| Orchidectomy | A short course of chemotherapy may be recommended depending on the risk of testicular cancer coming back. Alternatively, a programme of surveillance may be suggested to check for cancer on a regular basis. If there is any evidence that cancer has returned chemotherapy will be given to cure it. For early-stage testicular cancer men may be given both options and asked to decide which they would prefer. In this situation there is no right or wrong answer. | For seminoma only depending on risk factors. Used to kill cancer cells in the lymph nodes at the back of the abdomen. |
Emotions
Most people feel overwhelmed when they are told they have cancer, even if the chance of cure is very high. Many different emotions arise, which can cause confusion and frequent changes of mood. You may experience fear, resentment, and anger. Reactions differ from one person to another and there is no right or wrong way to feel. These emotions are part of the process that many people go through in trying to come to terms with their illness. Partners, family members and friends often experience similar feelings and frequently need as much support and guidance in coping.
Often the information that you will get at diagnosis will be overwhelming and you may not fully appreciate the implications of what has been said. As well as having to deal with your own feelings and fears, you may also find that a cancer diagnosis and treatment impacts on your relationships in unexpected ways, adding stress when you feel least able to cope with it. Whether at the point of diagnosis or after treatment being able to explore your concerns with someone who understands how challenging a cancer diagnosis can be will allow you to discover the best way to confront what has happened to you. Many treatment centres will have a team of specialist cancer counsellors who may be able to help men talk about their fears and worries during or after treatment. It is always a good idea to ask the specialist team if counselling is available.
Orchid currently offers a telephone counselling service. To find out more please click here

Patient Comments
After the ultrasound scan, I had several blood tests and then went to the consultant’s room, were the consultant said that I was going to have an operation to remove the testicle as they highly suspected that I had Testicular Cancer. I can still remember that point so clearly. He mentioned a fair number of different points but I was taken back completely by the word cancer. How was that possible 2 days after my 29th birthday. I had just moved away from my home town, moved to a new job and moved in with someone and now felt a very long way from my normal world. In fact I struggled to ask any questions although I had many. I was shocked and really angry, why all this now?
When I was diagnosed I didn’t want to it stop me planning things in the future. I knew I was going to beat it; I never let doubt creep into my mind. I wanted to get better as soon as I could. I know I had a good prognosis so I kept a positive look on it.
It was a very strange feeling and at the beginning I think I went into shock. It was all very quick as a few days after diagnosis I had the tumour removed and my body was changed forever. It was just torn apart and it was difficult to see any positives.
I returned home. In shock. Immediately on the internet doing research. I kept it quiet, not telling anyone. The next day I phoned my Dad to let him know. Hardest phone call I’ve ever made. It was during this phone call that I thought ‘These things happen’ and decided there was no point getting myself worried about it, I just needed to get on with it.

Reviewed 1/2024
Orchidectomy image courtesy of European Association of Urology
